Explaining the Types of Gynecomastia
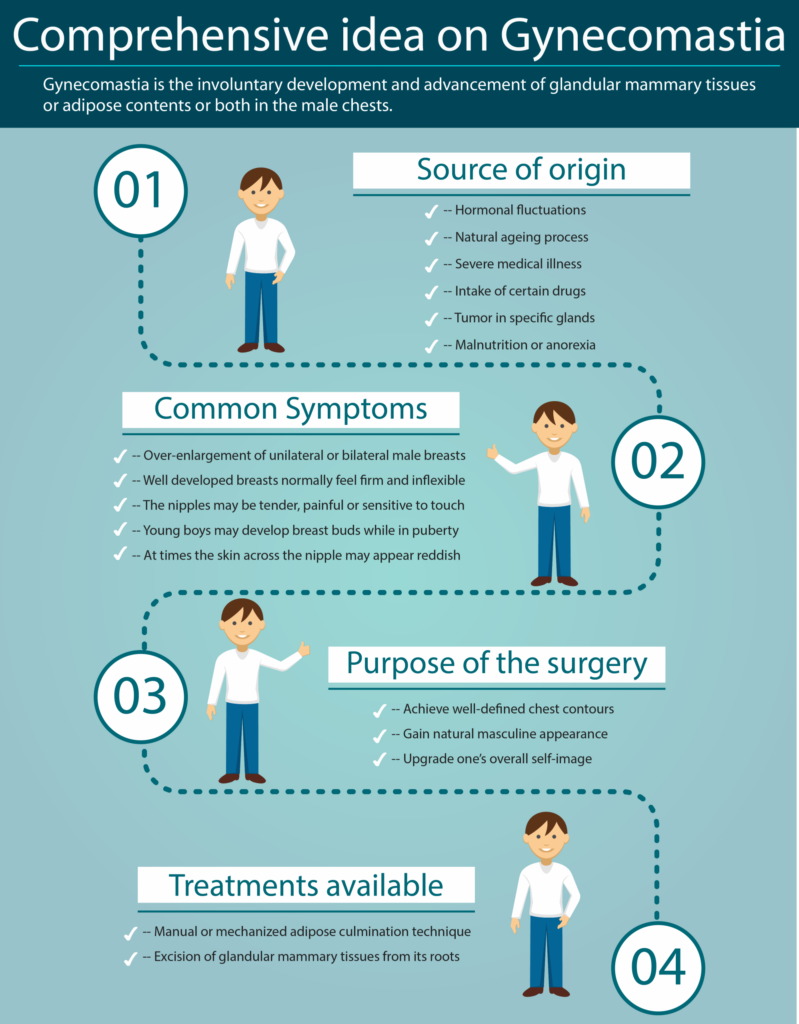
Gynecomastia, a glandular proliferation in the male breast, is a common clinical condition that may occur in males of all ages. “Gynecomastia” is derived from the Greek terms gynec (female) and mastos (breast) and was first coined by Galen in the second century AD. The condition may be an incidental finding on routine physical examination, or may present as new-onset palpable breast mass with or without discomfort.
While all forms of gynecomastia involve the enlargement of male breast tissue, the reasons behind it and its physical characteristics may vary. Here’s a breakdown of the various components that factor into the different type of Gynecomastia:
1. Pathological Gynecomastia
Gynecomastia can be classified based on histological types: florid, fibrous, or intermediate, with the type usually related to the length of the condition.
Three types of gynecomastia, florid, fibrous and intermediate, have been identified. The type seen is usually related to the length of the condition.
- Florid gynecomastia: This type is usually seen in the early stages of the condition, four months or less, and is characterized by increased vascularity and ductal tissue with loose and edematous stroma. This type of gynecomastia is characterized by an abundance of glandular tissue (the tissue responsible for producing milk in females) within the breast.
- Fibrous / Chronic dendritic gynecomastia : This type of gynecomastia is characterized by an irreversible excess of fibrous connective tissue and few ducts within the breast. Fibrous gynecomastia is typically seen after a year and can occur as a result of aging or hormonal imbalances. It can present as a rubbery or firm mass within the breast.
- Diffuse glandular or intermediate gynecomastia: This type of gynecomastia is a progression and falls somewhere between florid and fibrous gynecomastia in terms of its characteristics. It is often associated with chronic liver disease and can present as a firm, irregular mass within the breast. This type is commonly seen in patients receiving exogenous estrogen.
2. Physiological Gynecomastia
This type occurs naturally at different stages of life as a result of hormonal changes or imbalance and may resolves without medical or surgical intervention.
- Neonatal Gynecomastia: Many male infants experience temporary breast enlargement due to maternal hormones transferred during pregnancy. This typically resolves within a few weeks.
- Pubertal / Adolescent Gynecomastia: During puberty, hormonal fluctuations can cause temporary breast enlargement in up to 50% of adolescent boys. It often subsides within six months to two years as hormone levels stabilize. Also called (inaccurately, by the way) ‘congenital’ or ‘hereditary’ gynecomastia, this condition generally appears between ages 9 and 14 and may be seen transiently in as many as 30 to 50 percent of boys. In some cases, pubertal gynecomastia recedes with age, but about a third of all patients will have breast tissue that persists into their young adulthood, and improvement can only be achieved through surgical excision. Because pubertal gynecomastia can spontaneously regress, it is our practice policy not to provide surgical treatment for this group of patients until they are at least 16 years of age. There is evidence to suggest that adolescent gynecomastia is inherited.
- Adult Gynecomastia: In men over 50, declining testosterone levels and stable estrogen levels may lead to gynecomastia. This process happens as a result of an increase in aromatase activity. In other words, the brain, fat tissue, liver and testicles convert a larger portion of testosterone into estrogen. It is reported that after age 30, men lose 1% of their testosterone supply every year. By the time many men reach 75 they have lost 30% of the testosterone they had when they were 25. Factors such as weight gain, medications, or pre-existing health conditions can exacerbate the condition. Most cases of adult-onset gynecomastia, and some cases of adolescent gynecomastia, consist of a combination of enlarged breast tissue and an accumulation of fatty tissue. As the condition progresses, the male breast area becomes more and more feminized in appearance. However, unlike with gynecomastia stemming from puberty, gynecomastia during a man’s later years can be more severe and also permanent as there is not enough circulating testosterone to even out the sudden influx of estrogen. Many men will try to exercise excessively to rid themselves of the excess breast tissue, however even this does not work; as the excess tissue is most commonly glandular tissue and not fat.
3. Unilateral and Bilateral Gynecomastia
Gynecomastia can affect one or both breasts. The classification into unilateral or bilateral gynecomastia is visual and depends on whether one or both breasts are affected. Here’s a closer look:
- Unilateral Gynecomastia: This occurs when one breast enlarges more than the other, making it more noticeable. Gynecomastia typically presents as two-sided or “bilateral” growth, but in small percentage of men (less than 5-10%), it can present as single-sided “unilateral” or asymmetrical gynecomastia. Like bilateral gynecomastia, unilateral gynecomastia is a benign condition that is no different in terms of diagnosis and treatment. Unilateral gynecomastia is harder for men to deal with compared to the symmetrical or bilateral type. We really don’t know why some men develop unilateral gynecomastia. Some studies have shown unilateral gynecomastia associated with various drugs. For instance, oral Finasteride or “Propecia” used to treat male androgenic alopecia. Benign masses and cysts can also occur on only one side of the chest and are usually easy to diagnose by an experienced clinician. These are treated by surgical removal of the benign mass.
- Bilateral Gynecomastia: Both breasts are affected, either symmetrically or asymmetrically.
4. True Gynecomastia vs. Pseudo-Gynecomastia
Distinguishing between true gynecomastia and pseudo-gynecomastia is important, as the type of tissue involved can affect the treatment approach. Here’s what differentiates them:
- True Gynecomastia: In true gynecomastia, the glandular breast tissue under the nipple enlarges and feels firm. This type may require surgery for long-lasting results. ‘Puffy nipples’ or ‘pure glandular’ gynecomastia is a very common form of true gynecomastia, particularly in adolescents. The proliferation of breast tissue is limited primarily to the area immediately behind the nipple and areola, sometimes extending a short distance beyond. This creates a dome-like appearance of the nipple-areola complex. There is no associated proliferation of fatty tissue in the surrounding area. In most cases, this can be treated by simple excision of the retro-areolar breast tissue through a limited incision at the lower border of the areola.
- Pseudo-Gynecomastia: Pseudo-gynecomastia involves fat accumulation in the chest area with no real breast tissue growth. This is a very rare condition as most cases of chest fullness, involve enlargement of the breast gland as well. Liposuction is often the recommended treatment in such cases. In general, pseudogynecomastia accompanies an overweight condition in the entire body. Since the size of the chest will change with weight fluctuation, an enlarged chest caused by pseudogynecomastia can typically be resolved with weight loss and exercise. This is not the case for true gynecomastia. Many men with weight gain–related breast enlargement gradually develop some element of true gynecomastia as well. The condition of being overweight or obese can increase the relative ratio of estrogens to androgens that circulate in the bloodstream, which can trigger the enlargement of actual breast tissue. If pseudogynecomastia does not respond to diet and exercise, surgical liposuction is often recommended.
- Mixed Gynecomastia: We are in the midst of a nationwide obesity epidemic with up to 60 percent of Americans considered overweight or obese. We know that weight gain deposits fatty tissue throughout the body, including the male chest. The excess fat in the area of the hormonally sensitive tissue under the nipple-areola complexes causes an imbalance of the sex hormones, and this causes the growth of gynecomastia tissue. Unfortunately, weight loss does not result in the disappearance of gynecomastia as the tissue has become fibrotic and unresponsive to anything but surgery to remove the tissue. It should be known that this group of patients often have to confront the issue of skin removal treatment with scars across the chest at a much higher frequency because the stretched skin loses its elasticity. There is a convincing relationship between weight gain and gynecomastia.
Schedule a Consultation
If you believe you may be a candidate for gynecomastia surgery or would like to learn more about our services, we invite you to schedule an individualized in-person consultation and take the first step.
_____________________________________________________________
The Boston Gynecomastia Specialists is the premier Greater Boston Gynecomastia Center of Excellence. Our primary focus is on providing outstanding care throughout every step of your journey, from the first consultation to your full recovery. We recognize and appreciate the confidence you have in us and are unwavering in our commitment to maintaining the utmost level of patient care. Led by Dr. Edwin Ishoo, a highly skilled, board-certified surgeon with expertise and over 30 years’ experience in Male Breast Reduction, our dedicated team is fully committed to ensuring the best possible surgical outcomes tailored for each individual. Recognizing that every man is unique, we personalize our approach to meet your specific condition, needs and expectations. We welcome you to take that first step to achieving the transformation you have been imagining and contact the Boston Gynecomastia Specialists, the leading Gynecomastia Center in Boston, to meet with Dr. Ishoo for your personalized, in-person consultation and have your questions answered. Let us take the gynecomastia concern off your chest in a day and off your mind forever!